
Twenty-four-year-old Theresa moved from her hometown in Kwara State to the capital city of Abuja in search of greener pastures. She had hoped to get a job in the city, save money, and return to school. Armed with ambition and determination, she applied to several businesses for the role of a salesperson but was rejected at every turn. As the days turned into weeks and weeks into months, Theresa found herself confronted with the harsh reality of unemployment and resorted to sex work, first as a way to pass the time, then subsequently as a means of livelihood.
Four years after relocating to Abuja, Theresa’s life took a new turn. “I became very sick and was taken to the hospital, where I spent several days on admission,” she said. After undergoing several tests, she was eventually diagnosed with HIV. Theresa felt the ground shift beneath her feet as the weight of her diagnosis bore down upon her. “I was shocked to hear that I had HIV and would have to take medicine for the rest of my life,” she added.
Sex workers living with HIV are among the hard-to-reach key populations in HIV case management. They are often reluctant to visit health facilities for routine viral load tests for fear of discrimination and stigma. Following counselling from health workers, Theresa started receiving antiretroviral therapy (ART) and getting periodic viral load tests at a clinic in a remote community on the outskirts of the city, where no one would recognize her. For three years, she travelled to and from the community for her care and treatment. But as her health improved, the fatigue of frequent travel set in. With her resources dwindling, she could no longer afford the recurrent transportation fare to the clinic, so she started skipping appointments and eventually discontinued her routine treatment and viral load testing. Theresa’s situation represents the challenges experienced by thousands of key populations living with HIV, including Female Sex Workers, Men who have Sex with Men, and People Who Inject Drugs, who experience similar barriers to accessing vital laboratory testing services.
Laboratory services are a key component of a comprehensive health system, providing essential diagnostic services so patients receive appropriate medical care. With support from PEPFAR and USAID, the USAID Global Health Supply Chain Program-Procurement and Supply Management (GHSC-PSM) plays a leading role in helping countries expand and transform their laboratory services to be more cost-effective, efficient, and responsive to patient needs. In Nigeria, the Federal Ministry of Health established community-based one-stop shops to scale up HIV prevention, treatment, and care for key populations. These one-stop-shops cater to more than 79,000 recipients of care across 56 locations, and are designed to meet people where they are. “Instead of waiting for them to come to us, we move to the streets to counsel them, give them ART, and collect their specimens for viral load testing,” says Joffrey Okoeguale, the laboratory focal person at one of the community one-stop shops in Abuja.
However, transporting specimens collected on the streets to the laboratories was a significant challenge for Joffrey’s team. “We collected samples at night, and by that time, we can’t take them to the laboratories for analysis,” he added.
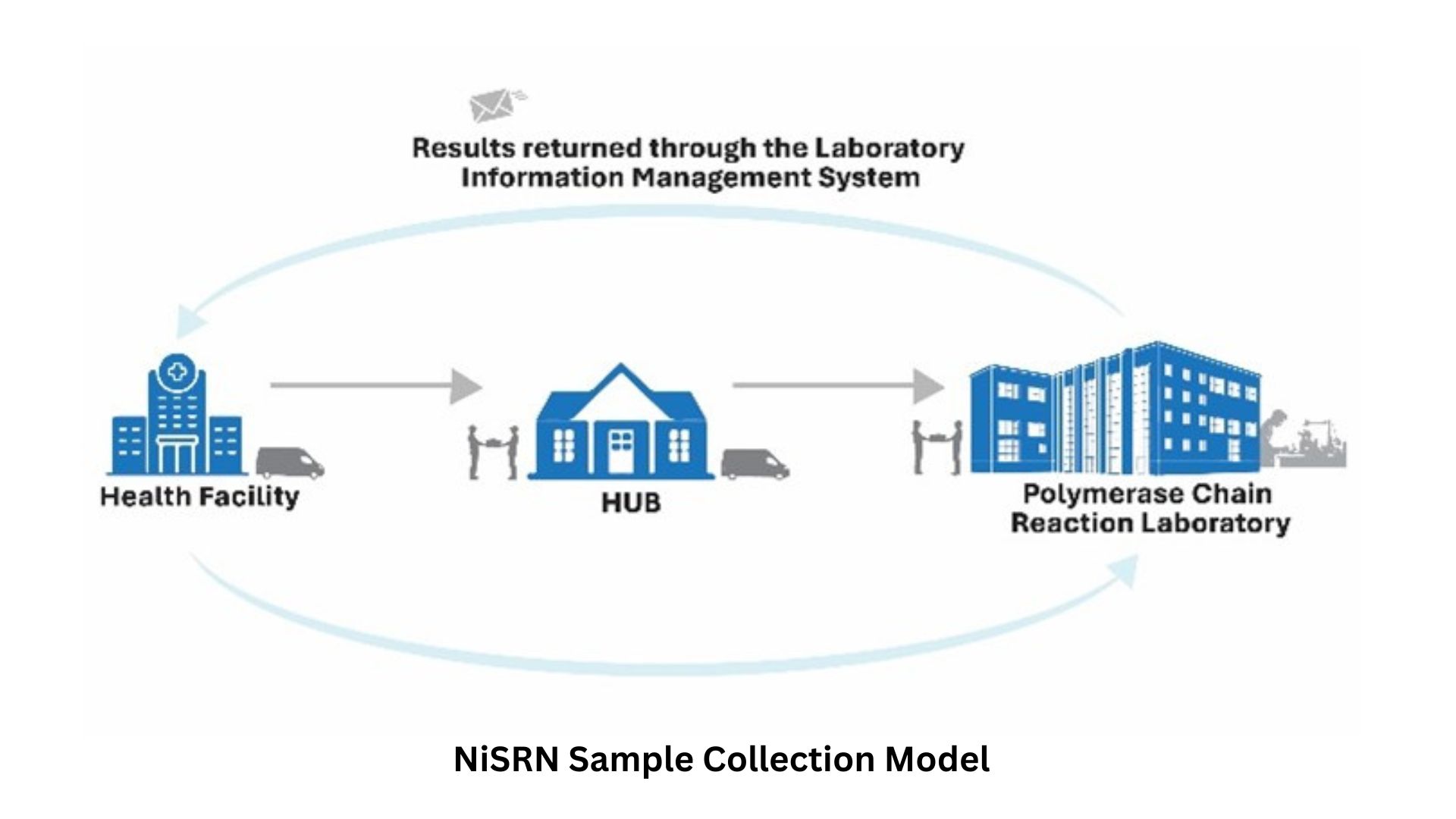
To address this challenge, the Nigeria Ministry of Health, with support from PEPFAR and the Global Fund, conducted a diagnostic network optimization exercise and established the optimized National Integrated Specimen Referral Network (NiSRN) as a solution to improving patients’ access to viral load, tuberculosis, and other laboratory testing services. As NiSRN began improving access to laboratory services, demand grew for reliable specimen transport services to move samples between the laboratories and points of care where patients were treated.
GHSC-PSM sought to meet this need by initiating a private-sector partnership with NiSRN. The project contracted third-party logistics companies that engaged motorcycle riders and transporters to implement a quick and efficient system for collecting and transporting patient specimens from collection centers to laboratories and transporting the results back to the requesting facilities. Through these actions, NiSRN ensures a responsive and agile routing of the samples via the primary and secondary lab arrangement and through bulk shipments to ensure that results are available in a timely manner for clinical decisions.

This coordinated system allows for more patient testing and improved viral load monitoring, especially for key populations and people living in remote areas. Between 2020 and 2024, NiSRN has facilitated the transport of over 333,000 specimen samples from one-stop shops to testing laboratories. Through these initiatives, the country is closer to achieving the third 95 goal, where 95 percent of all people on ART achieve viral suppression.
Optimizing the transport of patient samples is one of the five key components of GHSC-PSM’s network approach to strengthening and scaling up laboratory services. The ultimate impact of this laboratory network transformation is on the most important stakeholder: the patient. Since adopting this approach, more key population clients living with HIV have been reached and receive regular viral load monitoring.
This improved access has made life a little easier for Theresa, who no longer has to spend thousands of Nigerian Naira accessing ART and testing services. “This USAID initiative saves me the stress and time as I no longer have to travel to that remote village for tests and treatment. I feel much better,” she concluded.


